Implementing AI in healthcare RCM: How to build a structure for success 3 Apr 6:38 AM (15 days ago)
The healthcare industry is undergoing an AI-driven transformation, and revenue cycle management (RCM) leads the charge in many ways. As teams strive to reduce denials, increase cash flow, and streamline processes, implementing AI in healthcare RCM is essential.
In fact, organizations are already leveraging AI to:
- Eliminate 80% of manual work
- Increase point-of-service payments by 30%, and
- Rebill $5.9 million in missing charges.
What’s more, research finds that 92% of healthcare leaders say investing in AI, GenAI, and advanced automation for RCM is a top priority.
At Healthcare Information and Management Systems Society (HIMSS) 2025, Chris Schremser, Waystar CTO, spoke about this in-depth with Tiffany Trammel, IT Director of Revenue Cycle Systems at Cleveland Clinic. Their discussion shed light on how healthcare organizations can succeed in implementing AI in healthcare RCM while:
- Enhancing the patient experience
- Accelerating research, and
- Reaching operational efficiency.
Implementing AI in healthcare RCM
1. How to lay a foundation for success in AI
Structure + attention
To establish AI as a focus area, the healthcare organization introduced a Chief AI Officer in 2024. This was critical because it allows them to separate innovative AI initiatives from day-to-day IT operations, ensuring that both areas receive attention.
They also established a cross-functional AI committee to evaluate projects. With representatives from finance, research, IT, patient care, and strategy, the committee can:
- Streamline decision-making
- Mitigate potential conflicts among use cases
- Ensure all initiatives are strategically aligned
A key tool in this effort is their “build, buy, or partner” evaluation framework, which helps them decide which AI solutions should be developed (internal) or sourced (external) to maximize efficiency and effectiveness.
Education
The organization is also committing to AI education going forward by:
- Prioritizing foundational AI knowledge for all employees
- Focusing on deep AI knowledge for those in IT
- Developing educational roadmaps to keep staff informed long-term
Implementing AI in healthcare RCM
2. How to evaluate vendors for AI-powered RCM solutions
Vendor selection is a critical component of AI adoption, and successful teams often prioritize transparency. By choosing vendors that offer clear insight into their AI capabilities but are also willing to reveal their limitations, everyone stays on the same page. That’s become crucial recently with the rise of vaporware: software that is advertised as cutting-edge but isn’t ready or simply can’t deliver.
To avoid this, organizations should vet vendors to ensure all AI-driven solutions are:
- Functional: The technology is up and running, with performance metrics that show success
- Future-proof: There’s a maintenance and/or growth plan, ensuring the solution will evolve and improve
- Capable of integration: The technology can (or will) be used across the revenue cycle, not just at specific points
The third requirement — integration — is key. Rather than using isolated point solutions, organizations choose AI technology that can operate across workflows, which makes it possible to scale quickly.
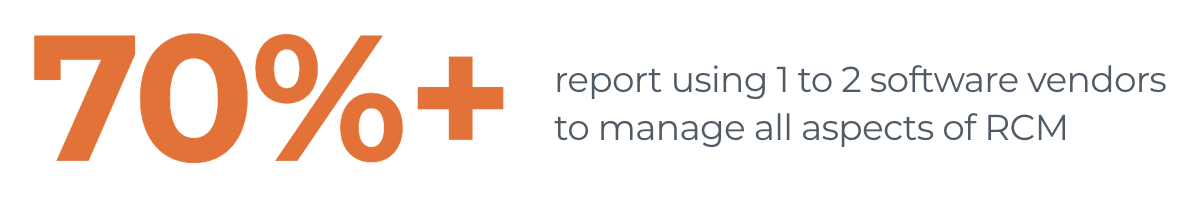
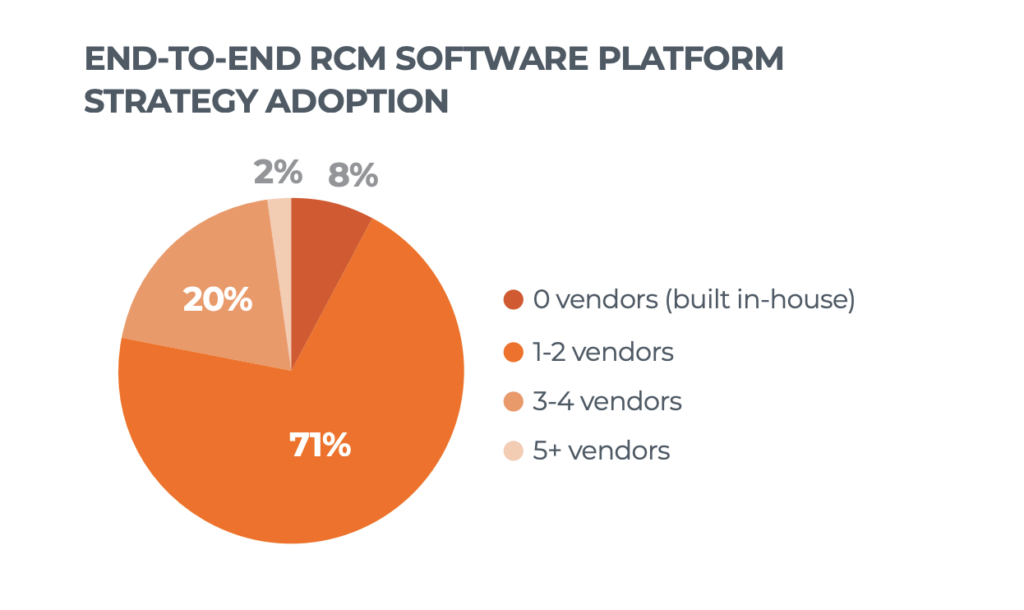
The pivot away from point solutions mirrors a larger trend in revenue cycle management: the move to end-to-end software. Studies show that 71% of healthcare leaders have 1-2 software partners managing their whole revenue cycle today. Just two years ago, roughly the same number (73%) were using 4+ vendors for RCM tasks. As the industry trends toward streamlined operations and selecting fewer partners more strategically, AI-powered solutions will be no exception.
Implementing AI in healthcare RCM
3. How to maintain + strengthen data security
As AI adoption accelerates, so do concerns about security and compliance. Even before the 2024 cybersecurity breach, leading organizations were taking action, partnering with the U.S. Department of Commerce to establish industrywide safeguards.
Today, organizations can maintain cybersecurity while deploying AI by:
- Evaluating vendors rigorously
- Sharing only essential data
- Employing a “human-in-the-loop” approach
The latter is critical to maintaining high standards for patient care and financial accuracy, especially in terms of identifying AI hallucinations: incorrect or misleading results that models generate due to errors or biases in training data.
Implementing AI in healthcare RCM
4. How to prepare for the future of AI in RCM
The healthcare revenue cycle industry is moving toward a future where AI is not just helpful but transformative. And leaders are already banking on that: 100% of healthcare leaders recognize the benefits of AI in revenue cycle management.
If your team is currently implementing AI in healthcare RCM, take a look at what’s working today so you can plan for tomorrow.
Take the next step with AI in RCM
- Unlock the top 6 trends in healthcare revenue cycle
- Examine AI + its ROI in healthcare payments
- See how Waystar clients are using generative AI to create appeal packages 3X faster
The post Implementing AI in healthcare RCM: How to build a structure for success appeared first on Waystar.
Top 6 trends in healthcare RCM: AI, ROI, data security + more 24 Mar 8:16 AM (25 days ago)
Today’s healthcare revenue cycle landscape is undergoing significant transformations. From shifting payer policies and skyrocketing denials to heightened concerns around data security, the challenges providers face grow more and more complex.
With $440 billion spent on healthcare administrative work every year, decision-makers are embracing new advancements in the healthcare revenue cycle — including artificial intelligence (AI), software innovations, and strategic partnerships — to drive efficiency and protect their organization’s financial health, now and in the future.
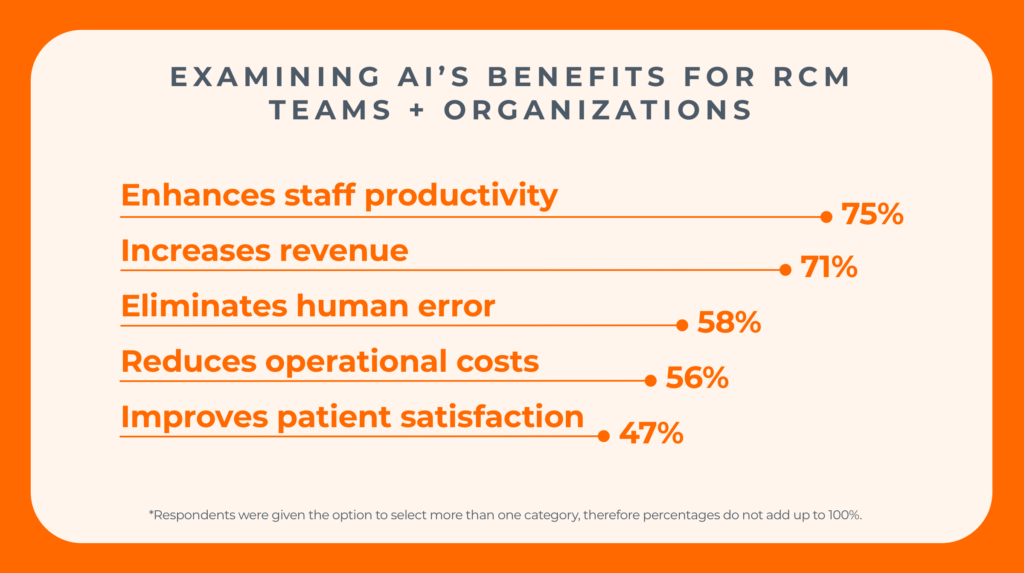
In collaboration with Qualtrics, Waystar conducted a recent market survey of more than 600 healthcare revenue cycle leaders, garnering exclusive insights that reveal the top investment priorities and strategic focus areas for 2025. Here are the top takeaways from the report — and ways your own health organization could see meaningful results.
TOP PRIORITY FOR RCM LEADERS
1. Investing in AI + GenAI capabilities to fuel efficiency + cost savings
In the healthcare revenue cycle, AI and generative AI (GenAI) are no longer just buzzwords — they are critical tools to maximize efficiency amid obstacles like rising transaction volumes and increasing costs.
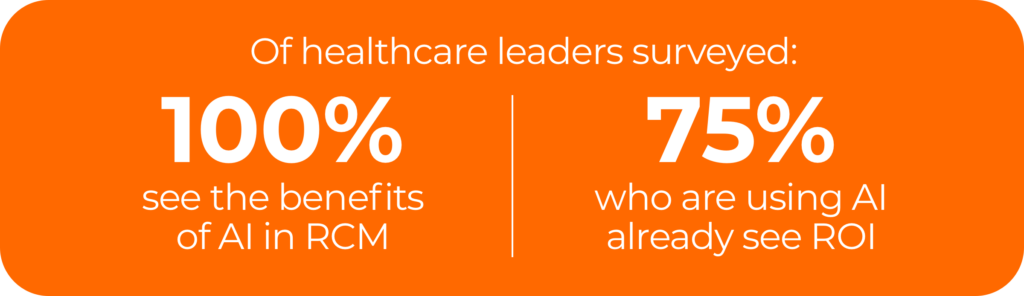
Survey data reveals that 92% of respondents indicate their top priority is to invest in or further implement AI, generative AI, and automation for revenue cycle management. Additionally, findings from a 2024 report show 100% of healthcare leaders see the benefit of AI in revenue cycle management.
Waystar recently launched AltitudeAI , a comprehensive set of capabilities designed to elevate productivity and precision for healthcare providers at scale. This includes Waystar’s own generative AI-powered innovation — AltitudeCreate
, a comprehensive set of capabilities designed to elevate productivity and precision for healthcare providers at scale. This includes Waystar’s own generative AI-powered innovation — AltitudeCreate — which launched within Waystar’s Denial + Appeal Management solution.
— which launched within Waystar’s Denial + Appeal Management solution.
This innovation has specifically enabled Waystar clients in the autonomous creation of appeal letters. Clients have already seen powerful results, including producing appeal packages three times faster, averaging 70% in time-savings.
WATCH NOW: The foundation and future of AI + generative AI in the revenue cycle industry
TOP PRIORITY FOR RCM LEADERS
2. Prioritizing RCM software that drives measurable ROI + financial performance
With so many industry pressures, it’s imperative to ensure that investments in healthcare payments software translate into tangible returns. According to survey results, 96% of providers consider strong ROI a top factor when purchasing new RCM software.
Furthermore, if current RCM software does not demonstrate desired outcomes or financial gains, healthcare leaders are quick to consider a new platform. In fact, software with low ROI ranks fourth in the top five reasons to switch to a new RCM partner.
“We know positive ROI is generated when we implement artificial intelligence,” said Chris Schremser, Chief Technology Officer of Waystar, during a 2024 keynote presentation The Foundation and future of AI + generative AI in healthcare payments.
With shifts in the healthcare revenue cycle landscape, AI and advanced automation remain powerful success factors to optimize financial performance and deliver long-term value.
CALCULATE NOW: See how much you could be saving with a platform approach to healthcare payments
TOP PRIORITY FOR RCM LEADERS
3. Safeguarding data against cybersecurity breaches
The February 2024 healthcare cybersecurity breach marked a turning point for revenue cycle leaders. After the most significant and consequential data breach in U.S. healthcare history, the protected health information (PHI) of 184 million individuals was compromised.
In the wake of this incident, safeguarding data and cybersecurity have become even more paramount for healthcare organizations. In fact, healthcare finance leaders cite data security concerns as a top reason they would consider switching RCM software vendors.
“You’ve got to have the critical infrastructure in place to be able to leverage data in a smart, responsible way. The underpinning of this is security; software providers must deliberately choose to secure their platform and be steadfast in achieving compliance,” shares Schremser.
WATCH NOW: Waystar security spotlight: A platform designed for trust
TOP PRIORITY FOR RCM LEADERS
4. Adopting end-to-end platforms over point solutions
Healthcare organizations are turning away from standalone solutions in favor of adopting end-to-end software platforms to address revenue cycle challenges. While relying on individual point solutions may have provided temporary relief in the past, they often lead to long-term inefficiencies and operational bottlenecks.
Research shows a 70% YOY increase in the adoption of end-to-end platform strategies. By shifting from fragmented solutions to end-to-end software platforms, providers can optimize performance across the revenue cycle, leveraging advancements in AI and automation.
With a platform strategy approach, data flows seamlessly from patient access to the final reimbursement, ensuring that all financial and clinical information remains accurate and consistent throughout the complete revenue cycle.
READ REPORT: Accelerate performance with an RCM platform strategy
TOP PRIORITY FOR RCM LEADERS
5. Enhancing patient access to boost precision + prevent denials
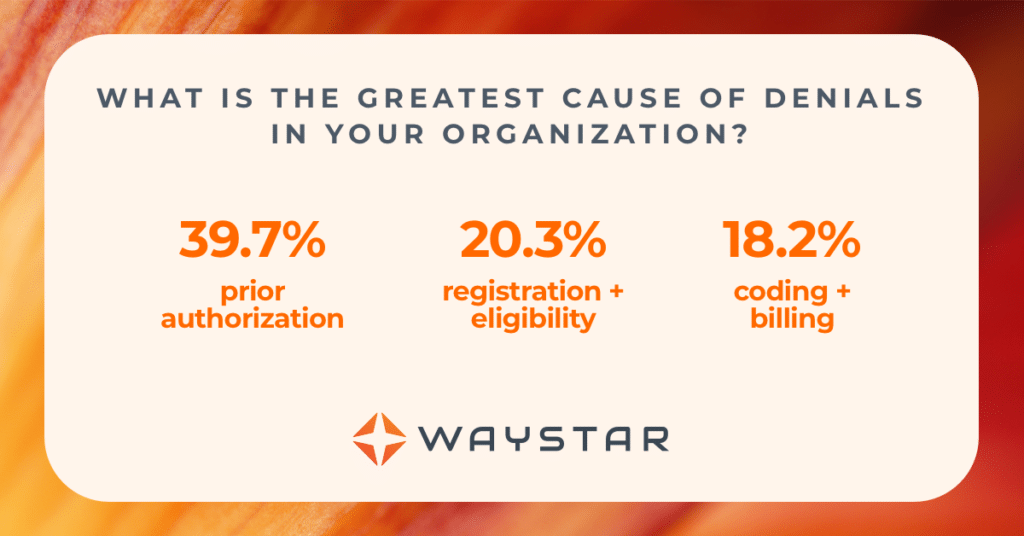
Every year, hospitals and health systems spend nearly $20 billion attempting to overturn denied claims. Furthermore, 60% of providers report their top pain point for denials stems from the frontend patient access processes, including prior authorization, registration, and eligibility.
Today’s providers understand that one of the most effect forms of denial prevention is ensuring upfront accuracy of all information at the beginning. Waystar’s Authorization Manager is helping healthcare organizations like Prisma Health improve authorization accuracy and speed.
“Prior authorizations are one of our biggest administrative challenges. By collaborating with industry partners on innovative processes that deliver high-impact solutions, we are able to make a significant difference for our organization and help provide better care for our patients,” shared Patrick Griffin, Executive Director of Revenue Cycle at Prisma Health.
EXPLORE MORE: How Waystar Authorization Manager increases speed and accuracy
TOP PRIORITY FOR RCM LEADERS
6. Strengthening cash flow with error-free claim submissions
When it comes to RCM functional areas, streamlining claim management to prevent denials continues to be a major focus. That’s because automating claim management workflows directly impacts a healthcare organization’s reimbursement speed, accuracy, and overall financial performance — along with their ability to fuel their mission.
With payers continually adjusting policies and procedures, automating claims is no longer optional. Leveraging AI and advanced automation in the claim management process ensures claims are submitted accurately the first time, leading to quicker reimbursements and stronger financial performance.
Explore the top trends in the healthcare revenue cycle for 2025
Read our latest report for RCM strategies to stay on the forefront of shifts in the healthcare payments industry.
The post Top 6 trends in healthcare RCM: AI, ROI, data security + more appeared first on Waystar.
Powerful AI: Examining results of Waystar AltitudeCreate™ in RCM 17 Mar 8:28 AM (last month)
There’s no denying that AI is changing the world — including the healthcare revenue cycle industry.
Today, revenue cycle leaders are seeking innovative solutions to improve efficiency, accuracy, and financial outcomes. Artificial intelligence (AI) has become critical in this transformation, and providers are increasingly turning to cutting-edge AI-powered solutions to streamline workflows and maximize revenue potential.
The integration of AI and GenAI within revenue cycle management is no longer a futuristic concept — it’s happening now. AI-powered solutions are helping providers reclaim lost revenue, accelerate reimbursements, and operate with a level of efficiency never before possible.
GEN AI RESULTS IN RCM
Accelerating appeal processes to combat denials
In January 2025, Waystar launched AltitudeAI , a comprehensive suite of AI-driven capabilities designed to enhance precision and productivity across the revenue cycle.
, a comprehensive suite of AI-driven capabilities designed to enhance precision and productivity across the revenue cycle.
One impactful component of this suite — AltitudeCreate — has already demonstrated significant improvements in Waystar’s Denial + Appeal Management solution by automating the creation of appeal letters. Early results speak volumes: AltitudeCreate
— has already demonstrated significant improvements in Waystar’s Denial + Appeal Management solution by automating the creation of appeal letters. Early results speak volumes: AltitudeCreate makes the appeal package creation process three times faster, saving 16 minutes per package (a 70% time reduction).
makes the appeal package creation process three times faster, saving 16 minutes per package (a 70% time reduction).

This rise of AI for the healthcare revenue cycle industry is fundamentally changing how organizations approach financial performance. Recent research shows that 100% of providers see the benefit of AI in revenue cycle management and 92% of providers intend to invest in advanced automation and AI for RCM in 2025.
The reason is simple: by leveraging advanced AI-driven technologies, healthcare organizations can reduce administrative burdens, improve accuracy, and expedite reimbursements — driving operational efficiency at scale.
GEN AI RESULTS IN RCM
Reach new heights in healthcare with Waystar AltitudeAI
AltitudeAI is built to empower providers with AI-driven capabilities that transform revenue cycle management. By tapping into Waystar’s robust data network, AltitudeAI
is built to empower providers with AI-driven capabilities that transform revenue cycle management. By tapping into Waystar’s robust data network, AltitudeAI delivers real-time insights and automation, allowing providers to achieve unparalleled accuracy, efficiency, and financial results.
delivers real-time insights and automation, allowing providers to achieve unparalleled accuracy, efficiency, and financial results.
With tools designed to anticipate challenges and proactively address inefficiencies, AltitudeAI drives meaningful outcomes across the revenue cycle.
drives meaningful outcomes across the revenue cycle.
- AltitudeCreate
 – Effortlessly generate content with AI-driven capabilities that enhance productivity and communication. Automated appeal letters reduce manual workloads and improve accuracy, enabling teams to focus on high-value initiatives.
– Effortlessly generate content with AI-driven capabilities that enhance productivity and communication. Automated appeal letters reduce manual workloads and improve accuracy, enabling teams to focus on high-value initiatives. - AltitudeAssist
 – Automate revenue cycle workflows with an AI-powered assistant that streamlines repetitive tasks. By increasing operational output, providers can allocate more resources toward patient care and strategic initiatives.
– Automate revenue cycle workflows with an AI-powered assistant that streamlines repetitive tasks. By increasing operational output, providers can allocate more resources toward patient care and strategic initiatives. - AltitudePredict
 – Anticipate outcomes and forecast trends using predictive analytics. Providers can proactively address potential denials, enhance financial planning, and navigate reimbursement processes with greater confidence.
– Anticipate outcomes and forecast trends using predictive analytics. Providers can proactively address potential denials, enhance financial planning, and navigate reimbursement processes with greater confidence.
The future of healthcare payments is here, and with the power of AI, providers can reach new heights in efficiency, precision, and revenue optimization.
Are you ready to transform your revenue cycle? Discover the power of AltitudeAI today.
today.
The post Powerful AI: Examining results of Waystar AltitudeCreate™ in RCM appeared first on Waystar.
RCM resource roundup: Activating AI for prior authorization + denial prevention 19 Feb 11:53 AM (last month)
Artificial intelligence (AI) is becoming increasingly essential in the healthcare revenue cycle.
Recent research shows that 92% of healthcare leaders cite AI and advanced automation as a top investment priority in 2025, particularly within patient access.
The reason is clear: 60% of RCM leaders say denials caused by errors in front-end, patient access processes are their top denial pain point — with the prior authorization space accounting for 39.7%. Therefore, investing in prevention is critical, and AI is proving to be the key.
In this blog, we dive deep into data, research, and real success stories to explore how healthcare teams are using AI for prior authorization — to ensure accuracy from the start.
SETTING THE STAGE
Get up to speed on AI + GenAI healthcare payments
Unpacking AI + GenAI in RCM
Get a simple explanation of the evolution of AI from machine learning to neural networks. Then, learn what AI and GenAI can do, from generating claim rules and appeals to monitoring payer behavior.
Modern Healthcare + Waystar report on AI + its ROI
To thrive, revenue cycle teams must leverage AI. But how are successful organizations doing it? What are the barriers to entry? And what’s the ROI? This comprehensive study offers answers.
Download study | Read blog | Watch webinar on demand
AI + GenAI email bootcamp
If you know you need to learn more about AI and GenAI but can’t find the time, join our bootcamp. We’ll deliver 1 email per week for 5 weeks in your preferred track:
Our beginner track (101) includes content like:
- A quick guide to AI, predictive analytics, and related terms
- 5 ways teams are successfully using AI in their revenue cycle today
- A simple explanation of generative AI and what it can do in RCM
Our intermediate track (201) includes a:
- Primer on GenAI from Waystar’s Chief Technology Officer
- Panel of experts discussing how to safeguard data while using GenAI
- Hospital discussing how they used AI to hit metrics like a 98%+ clean claim rate
WATCH + LEARN: ON-DEMAND WEBINARS
5 sessions on using AI in prior authorization + denial prevention
1. Hospital uses AI to boost revenue + slash denials
Hear directly from the leaders of Cincinnati Children’s Hospital about how they’re using AI to improve financial processes, make decisions, craft appeals, and eliminate 80% of manual work.
2. Diving into denial prevention with AI, appeals + more
Unlock a comprehensive plan for denial management and prevention that includes creating cleaner claims, responding to denials with data, and using AI to keep improving.
3. Q+A: How 1 health system overcame burnout + streamlined authorizations
Prior authorization processes are tedious and demanding. Learn how Lehigh Valley Health Network centralized authorization with AI and automation — saving 6,000 hours overall.
4. Securely leverage AI + machine learning to elevate performance
When 75% of health systems report positive ROI from AI investments, you need to know how they’re getting these results. Unlock specifics and learn how to do it all using best-practice security frameworks.
5. Q+A: Ask the revenue cycle experts — Claims, denials, AI + more
What are most revenue cycle professionals concerned about today? Watch this recording of our Q+A for answers about everything from denials and prior authorization to the future of AI.
PERFECT YOUR PROCESSES: EBOOKS
Streamline authorizations + implement AI-driven denial management
4 strategies to help your team + patients break through the billing haze
Explore tactics to enhance patient financial care, learn what to look for in automation and AI so your team can do more with less, and dig into case studies like Piedmont, an organization that:
- Automated 77% of manual AR follow-up work
- Increased point-of-service payments by 30%
- Generated $10+ million in payment lift
Crack the code: Recover more revenue with AI-powered charge capture
Discover methods for using AI and predictive analytics to improve charge capture, avoid underpayments resulting from inaccurate DRG assignments, and explore this technology in action by seeing how Aultman:
- Reduced costs by $3.3 million using AR automation
- Rebilled $5.9 million in missing charges
- Automated 25,000 AR transactions per month
ELIMINATE DELAYS + EXPEDITE APPROVALS
Activate advanced automation for prior authorization
Waystar Authorization Manager streamlines workflows, reduces manual work, and — with the introduction of Auth Accelerate — speeds up approvals so organizations like Prisma Health work smarter and get meaningful results faster.
To learn how your team can minimize rework and maximize results, schedule a demo today.
The post RCM resource roundup: Activating AI for prior authorization + denial prevention appeared first on Waystar.
Reimbursement roundup: Telemedicine, Medicare + reimbursement rate changes in 2025 11 Feb 7:15 AM (2 months ago)
Telemedicine and Medicare reimbursements are top-of-mind for healthcare organizations in 2025. With so many moving pieces, the changes can be difficult to navigate.
However, Dr. Elizabeth Woodcock shines a light on the complexities to help guide providers forward.
“For more than 30 years, I’ve been tracking what happens in the reimbursement and payment landscape,” says Dr. Woodcock, DrPH, MBA, FACMPE, CPC. “There’s a lot of change coming in 2025, and there’s no better time to talk about it than now.”

Telemedicine reimbursement in 2025: How organizations can prepare
Since the 1980s, patients have had to live in healthcare deserts for their providers to get reimbursed for virtual care. During COVID-19, the government expanded that access — but that expansion ends March 31, 2025.
“We’re at an inflection point for telemedicine,” says Dr. Woodcock. “There’s a law on the books for virtual care, and because the Centers for Medicare & Medicaid Services (CMS) can’t change the law, they’re still relying on regulatory power to keep telemedicine reimbursable.”
Think of it like a speed limit: If a road is under construction, the city can temporarily change the speed limit to keep people safe. But once that construction is over, the city can’t make that temporary change permanent; the government has to do it. That’s where we are with telemedicine.
Know what’s permanent: Telemedicine in 2025
Going forward, reimbursement will apply to telemedicine provided:
- By federally qualified health centers (FQHCs) and rural health clinics (RHCs)
- Using audio-only services if the patient can’t or won’t consent to video
- By clinicians using enrolled practice locations to provide care, even if the care is performed elsewhere (for example, from their home)
“If you’re a provider of telehealth in 2025, be sure to leverage virtual check-ins for patient interactions that don’t require an in-person visit,” says Dr. Woodcock. “These visits are reimbursable, and they help maintain patient engagement, improve efficiency, and capture revenue.”

Stay ahead of changes: Telemedicine in 2025
- Adopt the latest CPT codes + know payer protocol in your market
Despite virtual care’s uncertain future, the American Medical Association (AMA) has replaced phone-based codes for many services (audio-only visits, new versus existing patients). If you don’t use the proper CPT code, your reimbursement is at risk. - Know your state laws
Determine what services may revert to pre-COVID rules in your state. - Analyze the value of telemedicine for your organization
Consider reimbursement but also patient and provider satisfaction.
Medicare reimbursement rates in 2025: What providers need to know
Medicare reimbursement rates in 2025 are a major concern for healthcare providers.
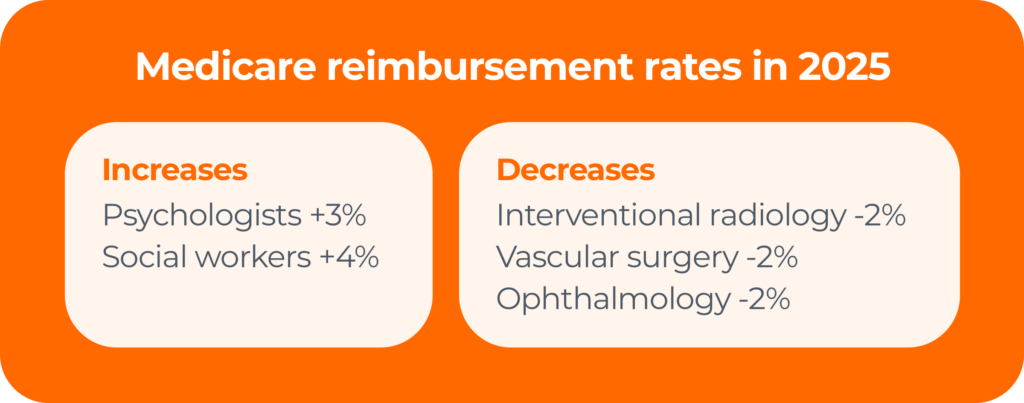
FACT #1: The Medicare conversion factor (CF) is down 2.83%
With the decrease from $33.29 to $32.35, providers are going to feel pressure, especially in settings where demand is high and care is scarce.
“This is bad news for us in healthcare,” says Dr. Woodcock. “There is an incredible supply-and-demand imbalance for provider services. There are so many waitlists, and nobody can get an appointment. That makes access to care really tenuous.”
There are a few winners for Medicare reimbursement rates in 2025 — psychologists and social workers — but there are also a handful of providers that use the same set of CPT codes that will experience a 2% decline. That includes radiologists, vascular surgeons, and eye doctors.
FACT #2: Physician reimbursements have been in decline for decades
An AMA study found that reimbursement for physician services has dropped by nearly one-third (33%) over the past 25 years. This decline has occurred despite the fact that the costs of running a practice — salaries, tech updates, compliance — have skyrocketed.
Medicare updates compared to inflation in practice costs (2001–2025)
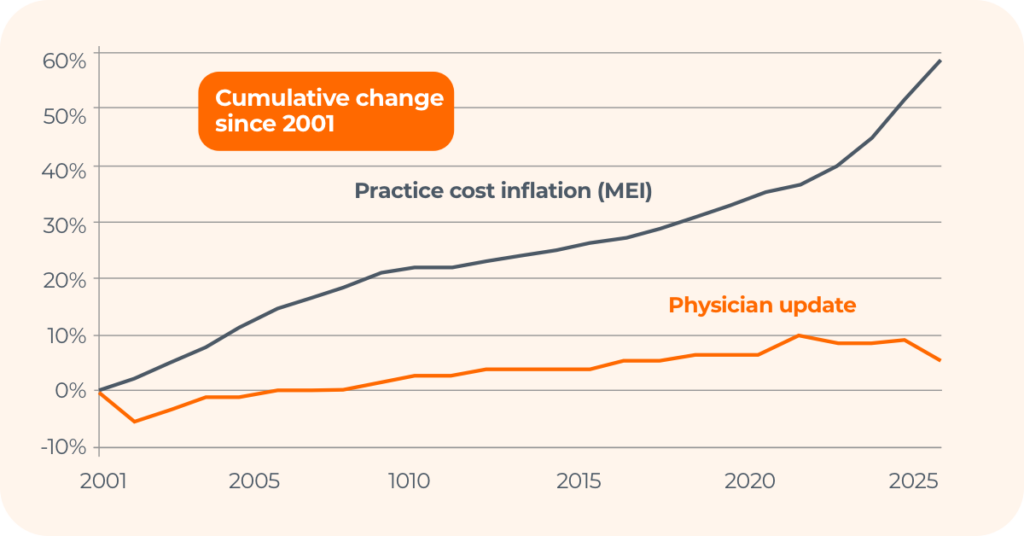
While there was a bill to counteract these cuts — the Medicare Patient Access and Practice Stabilization Act — it ultimately didn’t pass.
FACT #3: Sequestration will remain in place through 2030
Here’s a brief timeline of Medicare sequestration (the automatic, across-the-board spending cuts to federal programs):
- April 2013: Sequestration takes effect, reducing Medicare payments by 2%.
- May 2020 – March 2022: Congress suspends sequestration during COVID-19.
- April 2022 – 2025: Sequestration suspension is phased out.
Today, the full 2% sequestration is back in effect for all Medicare payments.
What can providers do?
- Use the Physician Fee Schedule search tool to see how these changes affect you.
- Consider diversifying your payer mix to reduce reliance on Medicare reimbursements.
Medicare services in 2025: What providers need to know
Medicare changes have ripple effects across the healthcare industry.

In 2025, Medicare reimbursements rates will increase for:
- Brain and mental health services, including FDA-cleared digital treatment devices
- Atherosclerotic cardiovascular disease (ASCVD) risk assessment and management
- Certain colorectal cancer screenings (CTC, blood-based biomarker)
- Hepatitis B vaccinations without an order
- Infectious disease care on the professional services side
5 steps to take to secure Medicare payments
- Consult the Medicare preventive services quick reference chart
Find out what’s covered, get related codes, track time limitations, and more. - Use CPT codes as much as possible
If you’re not using the proper CPT codes for services rendered, the codes may disappear. “CPT codes are use it or lose It,” says Dr. Woodcock. “Otherwise, what we’re signaling is that nobody is doing the work, and CMS will take them away.” - Claim payments for Advanced Primary Care Management (APCM)
If you provide primary care management for patients with one or more chronic conditions and meet certain requirements, use the following CPT codes to receive up to $110 per month per patient.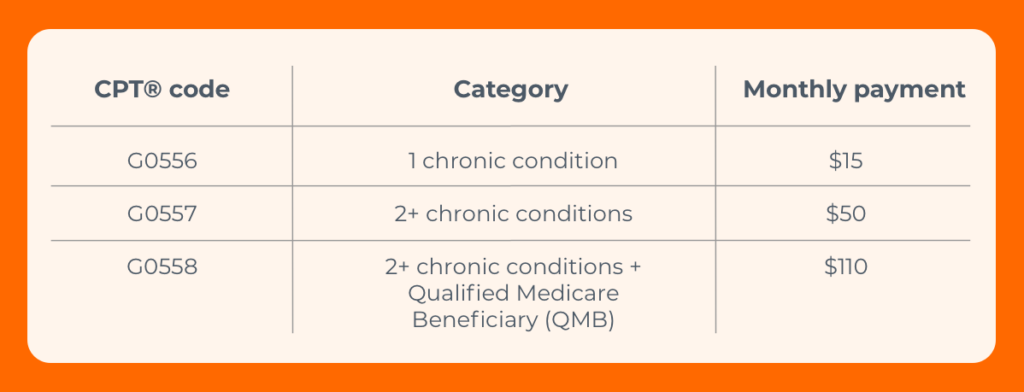
- Know where you stand with the Quality Payment Program (QPP)
- 2024 was the last year for any payment boost
- There have been changes to 66 current measures plus 7 new ones
- If you see CARC 237 or RARC N807, you could be penalized up to 9%
- Track changing and new CPT codes (including 270 new codes this year)
3 key takeaways for telemedicine, Medicare reimbursement rates + more in 2025
1. The healthcare industry is in the midst of massive changes
- Mergers and acquisitions are on the rise
Large health organizations will continue to grow, which affects the whole industry. - The physician shortage will get worse before it gets better
By 2036, the U.S. is projected to experience a shortage of 86,000 physicians according to the Association of American Medical Colleges. - The new presidential administration will heap change upon change
With new heads of both the Department of Health and Human Services (HHS) and CMS, change is the foregone conclusion.
2. The gateway to healthcare is now digital
“The front door to healthcare is changing,” says Dr. Woodcock. “It used to be us picking up a phone to call a provider. Today, it’s using digital tools that offer virtual health first. We’ve got ChatGPT, AI, Best Buy and Amazon Health, urgent care, and EHR systems that allow us to chat with our doctor without a copay.”

That’s leading to huge changes. Claim volumes are:
- Growing for retail clinics (200%) and urgent care (70%), but
- Shrinking for hospital ERs (1%) and primary care physicians (13%).
“What this means is we have to make sure we’re in the digital game,” says Dr. Woodcock. “We can’t go back and shut the door that COVID-19 opened. We’ve got to respond to our consumer.”
Make digital-first transactions work for you
Start with Patient Payments. Waystar clients have achieved a 30% increase in patient collections and 61% self-service pay rate on average using our integrated software.
3. Insurance payers still have the advantage
The pandemic tipped the scales in favor of payers.
“Claim volumes were lower during that time, but insurers didn’t reduce premiums,” says Dr. Woodcock. “So, patients continued paying while payers paid out less to providers.”
That’s still affecting providers today. Not only were margins low for years on end, but denials became an even bigger issue, with hospitals and health systems spending nearly $20 billion annually trying to overturn denied claims.
Stop the bleeding with automation, AI + GenAI to combat denials
When reducing denials is the #1 priority for providers, the right software is vital. See what Denial + Appeal Management can do for you, and how Waystar is leveraging generative AI to autonomously draft appeal letters with AltitudeCreate .
.
The post Reimbursement roundup: Telemedicine, Medicare + reimbursement rate changes in 2025 appeared first on Waystar.
3 top AI + GenAI advancements transforming RCM, denials + more 24 Jan 4:58 AM (2 months ago)
The U.S. healthcare system loses $350 billion to administrative waste annually, as denial rates continue to rise in number and complexity. In fact, estimates show that hospitals and health systems spend nearly $20 billion annually trying to overturn denied claims.
But providers are elevating productivity and precision with Waystar AltitudeAI to ascend toward their goals, while combating ongoing turbulent topics like rising denials, high costs, and surging transaction volumes.
to ascend toward their goals, while combating ongoing turbulent topics like rising denials, high costs, and surging transaction volumes.
That way, revenue cycle teams bring in fuller, faster payments for their organizations — and better care for their communities.
AI ADVANCEMENTS IN REVENUE CYCLE MANAGEMENT
Exploring the value + ROI of AI-powered software
Research has shown that AI has proven benefits in managing revenue cycle processes, from increasing accuracy and efficiency to bolstering the bottom line. In fact, 100% of healthcare finance leaders report that they see the benefits of AI in revenue cycle management.
Today, what may have once been considered beyond reach for revenue cycle teams is quickly becoming possible. Providers using AltitudeAI are empowered with new ways to prevent and combat denials, drive efficiency with AI assistance, and forecast trends for the future.
are empowered with new ways to prevent and combat denials, drive efficiency with AI assistance, and forecast trends for the future.
Despite the hype and attention AI is receiving, the technology itself is not new.
For more than two decades, Waystar has been continuously deploying and perfecting AI in our software platform. As leading experts in AI, software development, and the complex intricacies of the revenue cycle, Waystar is constantly inventing new ways to solve the challenges providers face every day in the U.S. healthcare industry.
Therefore, with each AI innovation — such as generative AI (GenAI) — Waystar has advanced beyond the curve, strategically and practically applying these enhancements in meaningful ways within our software.
On demand: Explore the foundation and future of AI + GenAI in healthcare payments >
AI ADVANCEMENTS IN REVENUE CYCLE MANAGEMENT
Practical applications of AI in denial management, appeals + more
Waystar AltitudeAI is available now to hundreds of thousands of Waystar providers and will expand to a million providers in the coming months.*
is available now to hundreds of thousands of Waystar providers and will expand to a million providers in the coming months.*
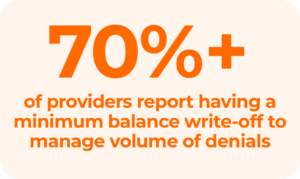
Although more than 50% of the 450 million yearly denied claims eventually get paid, the investment of time and resources to overturn these often causes critical delays in helping healthcare organizations get paid. Waystar is focused on simplifying labor-intensive processes and advancing applications for AI through:
- AltitudeCreate
 — Accelerate denial recovery and generate content effortlessly with AI-driven capabilities derived from a powerful data network. Tailored insights boost productivity with autonomous content and unprecedented accuracy to save both time and effort.
— Accelerate denial recovery and generate content effortlessly with AI-driven capabilities derived from a powerful data network. Tailored insights boost productivity with autonomous content and unprecedented accuracy to save both time and effort.
- AltitudeAssist
 — Drive efficiency by collaborating with an AI-powered assistant to streamline tasks. This empowers RCM teams to increase output, focus on high-value activities, and drive efficiency with intelligent automation for greater outcomes.
— Drive efficiency by collaborating with an AI-powered assistant to streamline tasks. This empowers RCM teams to increase output, focus on high-value activities, and drive efficiency with intelligent automation for greater outcomes.
- AltitudePredict
 — Remove uncertainties and make informed, proactive decisions by anticipating outcomes and forecasting trends. Navigate with precision through predictive analytics to achieve better clarity, combat denials, and accelerate payments.
— Remove uncertainties and make informed, proactive decisions by anticipating outcomes and forecasting trends. Navigate with precision through predictive analytics to achieve better clarity, combat denials, and accelerate payments.
With these AI and GenAI innovations, healthcare organizations can turn obstacles into opportunities in revenue cycle management to thrive in today’s operational landscape.
AI ADVANCEMENTS IN REVENUE CYCLE MANAGEMENT
Securely leveraging AI across the revenue cycle
Not all AI is created equal. The efficacy of the technology is only as good as the data it learns and gathers information from, making your choice of an RCM partner a critical decision.
The omnipresence of AltitudeAI across Waystar’s solution suites yields transformative capabilities derived from a powerful data network, enhancing data integrity and powerful results across the end-to-end spectrum.
across Waystar’s solution suites yields transformative capabilities derived from a powerful data network, enhancing data integrity and powerful results across the end-to-end spectrum.
In addition to maintaining the rapid pace of innovation, Waystar is equally focused on safeguarding data every step of the way.
That’s because, while nearly two-thirds of health leaders site data security concerns as a potential barrier for AI adoption, 89% also report that recent breaches haven’t changed their willingness to use AI in RCM.
Maintaining a strong security framework is critical to helping protect sensitive information while minimizing the risk of financial loss, data leaks, and security breaches.
Watch now: Learn about Waystar’s robust security framework >
Reach new heights in healthcare with Waystar AltitudeAI
Curious to learn more? Talk to a Waystar expert to discover how to harness these groundbreaking innovations for your healthcare organization today.
Speak to an expert
*Unlimited early access: Waystar AltitudeCreate innovations are available to applicable, existing, and newly implemented Denial + Appeal Management clients. Contact your client success manager or sales representative if you have any questions. Reach out to an expert.
innovations are available to applicable, existing, and newly implemented Denial + Appeal Management clients. Contact your client success manager or sales representative if you have any questions. Reach out to an expert.
The post 3 top AI + GenAI advancements transforming RCM, denials + more appeared first on Waystar.
How verifying insurance eligibility can increase revenue + ease staff burden 16 Jan 4:35 AM (3 months ago)
Note: This post was originally published in August 2022. It was updated in January 2025.
Verifying insurance eligibility can feel like a tedious, endless task. Without the right processes in place, staff spend countless hours on manual eligibility checks that drain time and resources. On top of this inefficiency, delayed or incorrect insurance eligibility verification can lead to:
- Missed reimbursements
- More uncompensated care
- Lower revenue
Why verifying insurance eligibility is pivotal when patients pay
Today’s patients are shouldering more of their care costs than ever before, and high or unexpected outstanding balances can negatively impact both their experience and satisfaction.
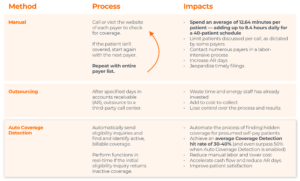
One big reason: Patients aren’t always up to speed on their current benefits and financial options, even when they actually have insurance coverage that could lighten their financial load. In fact, Waystar finds that 30-40% of presumed self-pay patients have some form of insurance, whether commercial, governmental, or a combination. The right coverage detection technology can find this insurance, allowing providers to collect a greater portion of care costs from payers — rather than patients — and increase point-of-care collections.
3 reasons real-time insurance eligibility verification matters
Timely insurance verification is crucial, as providers are far less likely to collect payment after a patient leaves the facility. Leveraging real-time solutions to verify insurance at the time of service has three major benefits:
- Enhancing revenue capture
- Easing the patient’s financial burden, and
- Streamlining the billing process from front to back.
How providers can find more coverage + collect fuller payment, faster
1. Take proactive steps to find hidden insurance coverage
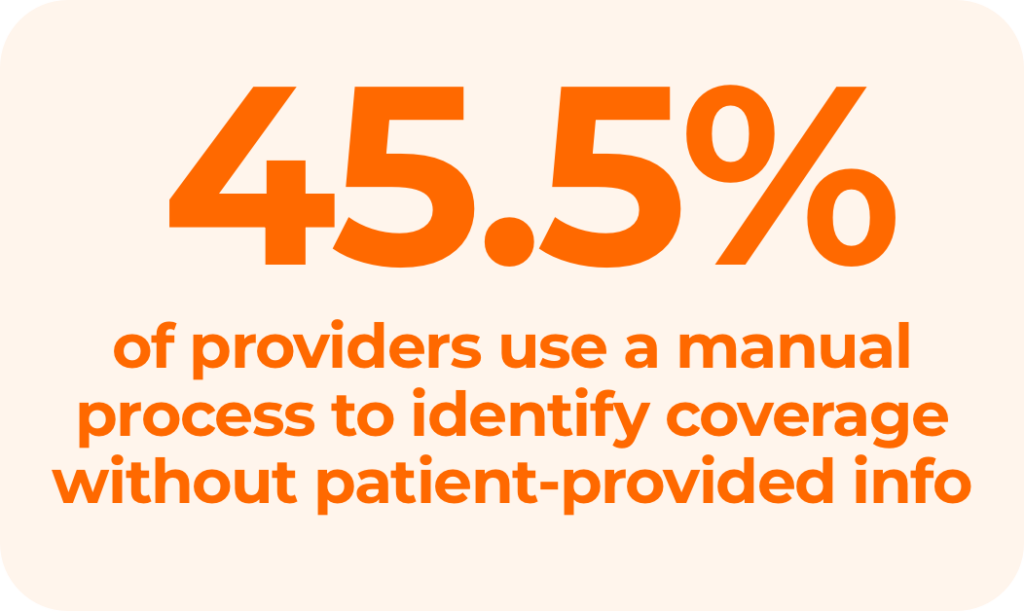
Without the right software, tracking down patients’ missing or unknown insurance coverage is time-consuming, costly, and involves multiple steps.
At the front end, patient access staff try to verify insurance eligibility before scheduled appointments. If they can’t, either the billing staff writes off the account, AR staff starts collections, or the account is outsourced to a third-party company for collection. Unfortunately, patient collection rates have decreased to 48% in recent years, increasing bad debt for providers and negatively impacting cash flow, revenue, and patient relationships.
An automated Eligibility and Coverage Detection solution that verifies active, billable coverage can empower your team to collect more revenue and lower bad debt. Leveraging these tools at the time of service can provide you with real-time information that can help you:
- Reduce denials
- Increase collections
- Boost cash flow
Methods for verifying insurance eligibility
2. Create a holistic strategy for patient communication and collection
Automated eligibility and coverage detection solutions can make a big difference in how much providers get paid — and how quickly.
Ineligible patient coverage is a leading cause of payer claim rejections and denials. But a coverage detection solution is really just one part of a larger strategy that can make life easier for your patients and your staff.
A proper holistic strategy considers how the solution:
- Works within your larger RCM framework
- Complements your patient engagement efforts
- Can improve or support other vital areas of your rev cycle, such as patient communications and estimates
With an automated solution, teams get critical financial information to patients as early as possible. A quick check using a coverage detection tool allows staff to find options the patient may not otherwise be aware of and even opens up an opportunity to collect from the patient at the point of service. Doing so ensures patients’ balance and financial responsibilities are presented in straightforward language.
Ask yourself: Would a patient need help to understand this bill or their responsibility? If the answer is “yes,” reconsider your strategy and your tools.
A holistic strategy will:
- Give patients convenience and flexibility in their payment options
- Streamline the collection process
- Reduce costs by saving your staff time, and
- Increase patient satisfaction and loyalty.
Ultimately, it’s those net benefits that will have the biggest impact on your bottom line.
Maximize revenue with insurance eligibility verification software
Waystar’s Coverage Detection solution can identify not only primary coverage but also help determine coordination of benefits when a patient has multiple health plans — and it can do both with simple information, such as patient name and date of birth.
This automated approach to insurance eligibility verification leads to the discovery of up to 40% more billable insurance, as well as:
- A reduction in collection costs
- Increased patient satisfaction and revenue
- More billable opportunities pinpointed by reporting and dashboards
- Optimized patient-collection workflows with automated batch and single-patient inquiries
- Real-time access to accurate insurance eligibility and coverage details
Learn about finding more coverage for patients, automating your insurance detection processes, and calculating your organization’s potential savings and annual recoupment.
The post How verifying insurance eligibility can increase revenue + ease staff burden appeared first on Waystar.
Coverage Detection 101: How RCM teams find missing or hidden insurance 15 Jan 1:41 PM (3 months ago)
Note: This post was originally published in August 2022. It was updated in January 2025.
When it comes to coverage detection, how much insurance is slipping through the cracks?
As medical plans become increasingly complex and ambiguous, patients and providers face challenges. Many patients are confused by their coverage, or unaware they have it at all. For staff, limited bandwidth and the lack of supporting tools — in addition to receiving inaccurate information from patients — make it difficult to bill the right payer first or know when to collect from the patient.
Your organization likely has its own strategy in place to identify patient coverage and work through obstacles. However, if you’re using an inefficient or highly manual process, you could be letting crucial dollars go uncollected.
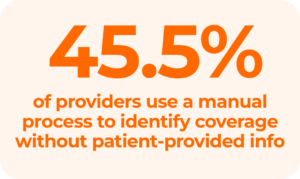
What is manual coverage detection costing you?
Relying on staff to find active insurance manually can drain resources and slow down your revenue cycle. Consider these challenges:
- High costs and inefficiency: Tracking down missing or unknown insurance is time-consuming, expensive, and high-touch
- Increased denials: Hidden or inaccurate coverage is a leading cause of denials, delaying reimbursement and extending days in AR
- Human error: Trying to find active insurance by phone or online increases the risk of errors and likelihood of overlooking billable coverage
- Burden on staff: Manual verification adds administrative pressure, especially with staffing shortages at an all-time high
Is hidden coverage creating more bad debt?
With out-of-pocket costs rising, many providers say they have written off expenses to cover the cost for patients who cannot afford to pay their bills. Without insurance, much of what is owed by self-pay and uninsured patients is never realized. However, a pattern of uncompensated care can have a major effect on your bottom line and even negatively impact the patient experience.
Many self-pay and uninsured patients have hidden medical coverage that you — and they — are unaware of. In fact, up to 40% of self-pay patients have full or partial coverage that they know nothing about.
How does this happen?
- Some patients may be covered by more than one insurance company or government agency
- Others may qualify for charity care, disability coverage, or workers’ compensation, providing alternative ways to lessen their financial burdens
Get compensated for care
Educating patients about their coverage and having transparent discussions about cost goes a long way to gain trust. Combining these conversations with smart automation ensures you capture every opportunity to identify billable insurance.
Are self-pay and uninsured patients impacting your bottom line?
Did you know that it’s twice as expensive to collect from patients as from payers? According to recent CDC data, millions of people across the country lack insurance coverage.
But advanced technology can help RCM teams:
- Find missing or hidden coverage in real-time, before the patient leaves the building
- Resolve self-pay accounts in-house, eliminating the need to outsource
In addition to helping patients, this will also give you more control over collections, save time, and decrease days in AR.
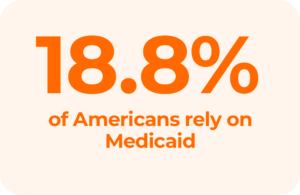
How seamless is your Medicaid claims process?
Nearly 19% of the U.S. population relies on Medicaid, which can introduce unique challenges. As a best practice, your team can consider Medicaid as the payer of last resort, making sure to investigate all other coverage options first.
Why? If Medicaid is filed when other coverage exists, it costs your organization time and money to process the claim — just to have it rejected. With fewer days left for re-processing within the timely filing window, inappropriately billing Medicaid can also add extra costs to the process and reduce revenue, causing a double hit to your revenue cycle.
Find coverage before filing Medicaid
Rich payer connections and smart technology can help you navigate the complexities of Medicaid and maximize your returns. At Waystar, we leverage more than 1,200 payer connections through our platform to surface hidden coverage in more cases.
<h2class=”mt-4″>Are you using the right tools to boost efficiency + minimize manual work?
In addition to inefficiency, the wrong tools can lead to missed opportunities and slower cash flow. Switching to an automated solution offers benefits including:
- Real-time insurance detection: Verify eligibility and uncover coverage instantly to minimize delays
- Improved efficiency: Purpose-built automation reduces administrative burdens, allowing staff to focus on tasks requiring human intervention
- Accelerated reimbursement: Streamlined processes lead to faster collections and fewer denied claims
Team up with a partner who delivers precision, accuracy, and results.
Does your current vendor check these boxes?
- Utilize extensive, accurate data rather than rely on limited or outdated third-party databases
- Provide a confidence rating for coverage results so your team doesn’t waste time double-checking
- Enable pre-claim coverage detection to ensure claims are accurate before submission
- Offer real-time coverage detection to identify billable coverage at the time of service
- Automate coverage detection across the revenue cycle to reduce denial risk at every stage
Calculate: How does your organization measure up?
Use our Coverage Detection calculator to see how much you could save in minutes. Uncover hidden revenue and put these strategies into action with the power of Waystar’s Coverage Detection solution — so you can focus on what matters most: caring for patients.
The post Coverage Detection 101: How RCM teams find missing or hidden insurance appeared first on Waystar.
6 key milestones that advanced Waystar’s mission in 2024 12 Dec 2024 7:47 AM (4 months ago)
For everyone in healthcare revenue cycle management, 2024 was a year of facing unprecedented challenges and rising to the occasion.
From navigating an industry cyber event to embracing the rapid evolution of generative AI, revenue cycle teams have delivered care to patients throughout a tumultuous year — while still streamlining the payment process.
“We’ve never had more technology than we do right now to tackle our most difficult payment challenges,” says CEO Matt Hawkins. “If Waystar can help providers find even five more minutes for a patient, we all win.”
Here are some monumental strides Waystar took in 2024 on our journey to simplify healthcare payments.
Waystar’s 6 major milestones of 2024
1. Elevated software with innovations in generative AI
Waystar has been using AI and machine learning (ML) for over a decade, building neural networks to achieve deep learning and ultimately create something new.
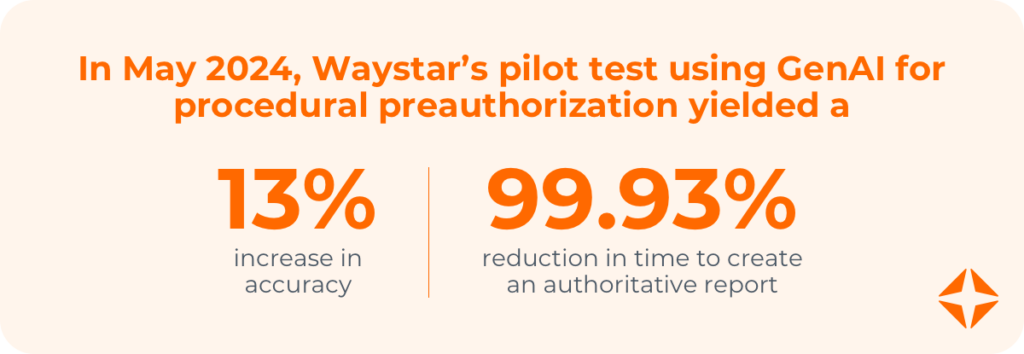
In 2024, Waystar collaborated with Google Cloud to use GenAI to automate the extraction of prior authorization requirements from complex payer data sets. In a proof-of-concept study, Waystar was able to improve accuracy by 13% and productivity by 500%.
“Google has a large language model (LLM) that’s specific to medical terminology, and Waystar processes over 5 billion insurance transactions every year,” says Hawkins. “Generative AI capabilities tend to benefit from large data sets. So, pairing their LLM with our data, we can unlock power for our clients, reduce errors, and create a more intelligent platform.”
Additionally, Waystar teamed up with Modern Healthcare to launch Examining AI adoption + ROI in healthcare payments, a research study exploring how healthcare leaders are navigating the impacts of AI in RCM — and what they plan to do about it for their own organizations.
2. Welcomed 30K+ providers amid a major cyber event
On February 21, a cybersecurity breach compromised the data of 100 million people. It was an unprecedented, challenging time for everyone in the industry, and one that required an immediate response.
“At Waystar, we quickly focused our efforts and marshaled additional resources to help impacted providers simplify their healthcare payments and regain cash flow,” says Hawkins. “We are pleased to report that Waystar has helped more than 30,000 providers move rapidly to the Waystar software platform — many in as little as three days — to minimize their disruption during this time and to get paid for the healthcare services they delivered.”
Through the Accelerated Implementation Program, health systems joining Waystar submitted tens of millions of dollars of claims within two to three days.
“We’re grateful that Waystar was in a position to help,” says Hawkins, “but that work is still going on today, especially when it comes to investing in our platform and being proactive in terms of security.”
3. Enhanced cybersecurity measures to safeguard data
In today’s ever-evolving cyber landscape, Waystar remains committed to proactively safeguarding clients’ data and securing its software platform. Waystar utilizes a robust framework for cybersecurity to monitor, measure, and mitigate risk, and includes:
- Conducting regular HITRUST, PCI, SOC II, and NIST audits
- Enforcing rigorous cybersecurity protocols
- Ensuring system resiliency and 24/7 monitoring
“It’s nothing new to say that, at Waystar, we focus on our clients. We work with over a million providers across all care settings, and we believe the key to serving clients is continued innovation, secure software, and trust,” Hawkins says.
“Whether we’re taking our team through a NIST Cybersecurity Framework (CSF) or implementing suggestions about client care from our advisory board, we feel a tremendous accountability to our clients,” adds Hawkins.
4. Collaborated with the Waystar Advisory Board
The Waystar Advisory Board is a network of leading healthcare executives representing top provider organizations nationwide. The board meets regularly to discuss revenue cycle challenges and advise Waystar on solutions to chart the path forward.

 .
.“We’re grateful to have this impressive group contribute their time and wisdom to advocate for Waystar,” says Hawkins, “and we’re grateful to be able to incorporate that thought leadership into our strategy, product roadmap, and client experience.”
5. Hosted the second annual Waystar True North client conference
client conference
In September, hundreds of providers of healthcare RCM services met for the annual Waystar True North Conference.
Conference.
Over three days, Waystar clients talked about everything from GenAI and preventing denials to safeguarding data. Through dozens of sessions, workshops, and events, attendees walked away with CEU credits as well as new connections and memories.
“We don’t do a lot of ordinary things at Waystar,” says Hawkins. “We try to create special interactions and special connections. Seeing the peer-to-peer idea sharing, innovation, and friendships forming every year at Waystar True North is one of my new favorite things.”
is one of my new favorite things.”

 2024.
2024.6. Launched an IPO on the Nasdaq Stock Exchange
In June, Waystar launched an initial public offering (IPO) on the Nasdaq Stock Exchange.
“The most exciting part of going public for us is getting the chance to tell our story to a bigger audience,” says Hawkins.

“Waystar’s message has always been a disruptive one — we’re not here to kick the can down the road or maintain the status quo. We’re here to ask, ‘What’s possible? How can we create software and stand up for providers?’ That’s what we’ll continue to do.”
Going public also reinforced Waystar’s credibility and impact.
“We were audited by leading financial institutions and technology experts, and we were able to prove that we are well governed by a strong, independent board,” says Hawkins.
With the proceeds from the IPO, the company is able to further invest in advanced innovations and enhance client experiences.
Still feeling shockwaves with your healthcare RCM services?
After everything that happened in 2024, many providers are still rebounding. Access our most-viewed resources on cybersecurity, support, partnership, and more for a one-stop guide to get ready for 2025 (and beyond).
The post 6 key milestones that advanced Waystar’s mission in 2024 appeared first on Waystar.
Revenue cycle 101: AI + generative AI in healthcare payments 6 Dec 2024 8:41 AM (4 months ago)
Generative AI in healthcare payments is top of mind for revenue cycle leaders. In a recent study, 90% say they plan to invest further in AI soon.
But how many RCM professionals fully understand how AI and GenAI impact healthcare payments?
“It’s okay if you don’t!” said Chris Schremser, Waystar’s Chief Technology Officer, at the 2024 Waystar True North client conference. “We shouldn’t be shy when it comes to asking questions about artificial intelligence or GenAI. It’s the only way to uncover what’s possible — and then put those innovations to work.”
client conference. “We shouldn’t be shy when it comes to asking questions about artificial intelligence or GenAI. It’s the only way to uncover what’s possible — and then put those innovations to work.”
In his session — The foundation and future of AI + GenAI in healthcare payments — Schremser covered:
- Key findings from the Waystar + Modern Healthcare report on AI and its ROI
- How organizations are using AI to:
- Maximize reimbursement
- Improve efficiency
- Prevent denials
- Enhance patient financial care
- Use cases for GenAI, including:
- Claim rule generation
- Medical necessity evaluation
- Monitoring payer behavior
- Infrastructure requirements for successful GenAI in healthcare payments:
- Technology
- Data
- Expertise
- Execution
Critically, Schremser also offered a simple explanation of the evolution of AI in healthcare payments, as well as four key facts RCM teams need to know now.
Watch (or listen to) the session on demand or read on for a primer.
The evolution of AI + GenAI in healthcare payments
Most healthcare finance leaders who are using AI have seen positive returns.
“AI leads to smarter decision-making, faster execution, and fewer errors,” says Schremser. “Generative AI allows us to take tasks that were historically impossible and make them very hard. Make no mistake — these things are still really, really hard. But they are now possible, and that’s the distinction.”
How does generative AI in healthcare payments work?
In the simplest terms, these technologies build on one another.
When all the different pieces of AI work together correctly, we can get machines to:
- Work like humans to complete tasks automatically (artificial intelligence)
- Identify patterns in data and make predictions (machine learning, neural networks)
- Decide if their predictions are right or wrong and make changes (deep learning); and
- Create new content with little to no human intervention (generative AI).
4 key facts about AI + GenAI in healthcare payments
In addition to discussing the evolution of AI in healthcare payments, Schremser revealed Waystar’s 2025 roadmap and these critical truths:
- If you train a model on bad data, you get bad results.
- It will never be cost-effective to use GenAI to solve small problems.
- Efficient AI only involves humans for review, verification, or complex issues.
- If GenAI doesn’t show ROI, it’s a waste of time.
“The truth is generative AI is really expensive, so if we’re using it to solve small problems, we’re wasting our time,” says Schremser. “But, if we can use GenAI to create things we can review, edit, and approve — while the system checks everything else in the background — the return on investment is high.”

The post Revenue cycle 101: AI + generative AI in healthcare payments appeared first on Waystar.